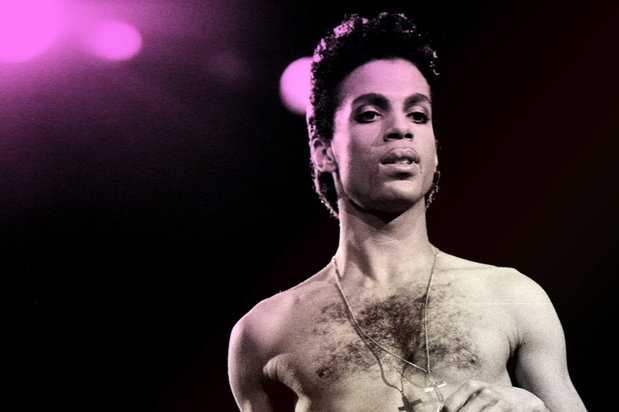
It’s been over a month since Prince’s passing and the world is still mourning the death of the Purple Legend. After a whirlwind of media speculation, the Associated Press has officially reported today that the singer died of an opioid overdose.
According to court records, Dr. Michael Schulenberg, a Minneapolis-area doctor, and Dr. Howard Kornfeld, a nationally recognized opioid addiction specialist, were both called the day before Prince’s death. Since Howard was not able to clear his schedule, he sent his son, Andrew Kornfeld, on his behalf with a small amount of buprenorphine. This drug could have potentially saved Prince but, unfortunately, Andrew arrived hours too late.
What is Buprenorphine?
Buprenorphine is an opioid agonist prescribed to help people reduce or quit the use of highly addictive opiates such as heroin and opioid painkillers. Typically sold under the trade name Suboxone, buprenorphine binds to the same opioid receptors in the brain but doesn’t produce a euphoric high. It is primarily used in medication assisted treatment and may be administered in the physician’s office or prescribed for take-home use. Additionally, it can help stabilize a person experiencing opiate overdose.
Compared to methadone, which was once the standard for treating opioid and opiate addiction, the most common form buprenorphine therapy also poses lower risk for abuse. But despite its strong role in helping patients with addiction, strict U.S. drug regulations have long thwarted the drug’s potential to make a dent in the addiction crisis.
Federal Regulations and Other Barriers for Widespread Use
In the U.S., buprenorphine is classified as a Schedule III controlled substance and is rigorously monitored by the Drug Enforcement Administration (DEA). Therefore, in order to prescribe the drug, physicians must obtain a DEA waiver, complete special training and comply with the limits set for the number of patients treated with buprenorphine. Due to all this red tape, an estimated 53 percent of U.S. counties are left short of physicians certified to prescribe the drug.
Dr. Thomas Kosten, a professor and the Jay H. Waggoner Chair in the Psychiatry and Behavioral Sciences Department at Baylor College of Medicine in Houston, says the reason behind the DEA’s tight limitations is to prevent a repeat of the street diversion and abuse that occurred back in the early days of methadone maintenance. “The patient number limitation provides an easy way for the DEA to prosecute such MD’s who might try to establish similar ‘medication mills’ for buprenorphine,” he explains.
While these regulations sound good in theory, their implications look more complicated on the ground. Kosten says that many physicians are simply not interested in treating a large number of patients whose primary reason for treatment was addiction. “These MD’s are afraid of the unknown qualities of the primarily addicted, as compared to their own patients with comorbid depression, diabetes, back pain, migraines or other more mainstream medical problems that brought them to [addiction] treatment,” he says. In Buprenorphine Prescribing: To Expand or Not to Expand, a study conducted by Kosten and his colleagues, research indicates that only 44 percent of U.S. physicians have obtained the certification required, with each of those prescribers treating less than five patients.
Another impediment for its widespread usage includes people in recovery who view buprenorphine therapy as addiction switching. The controversy lies in the fact that buprenorphine is an opioid drug, making its use non-conducive to abstinence. Kosten argues that this doesn’t discount the benefits buprenorphine can bring to those who are currently self-medicating. “The risks of death and disability to the patient and the harm to society are considerably reduced with buprenorphine compared to using heroin or other illicit opiates from the street or from doctor shopping,” Kosten says. “The withdrawal symptoms are [also] less severe than from other opioids and last about seven days after discontinuation.”
Tackling the Opioid Epidemic in 2016
For a long time, officials have erred on the side of caution when it came to buprenorphine, and rightfully so. Insofar, research has shown that an increase in buprenorphine therapy also causes the drug’s abuse and diversion rates to spike—as inevitably is the case with any drug intended to treat addiction.
But as the opiate crisis ensues and tragedies like Prince's passing bring more light to the issue, the U.S. is starting to strategically address what has become the leading driver of drug overdose deaths in the country. Kosten, who has published over 650 papers, books, and reviews regarding the treatment of addictive disorders, believes that what our nation needs is thoughtful planning and coordination. “This problem can be readily managed by a combination of professional education about prevention of addiction and management of pain without opioids, and FDA and DEA regulation of opioid prescribing.”
With 2016 being an election year, many politicians are promising to make headway on tackling the opioid crisis. This year, the senate has passed bills such as the Comprehensive Addiction and Recovery Act of 2016, which has designated $80 million in advancing treatment and recovery support services across the country. In March, the Center for Disease Control issued stricter guidelines for primary doctors when prescribing addictive opioid painkillers for managing chronic pain. And President Barack Obama, within his last year in office, has also made moves on the treatment front as he recently announced an initiative intended to expand access to drugs proven effective against opiate addiction, including buprenorphine.
These, however, are just baby steps toward a long and arduous journey. On top of public policy, providing assistance to those who are out to make a difference and giving those in addiction the opportunity to decide if medication assisted therapy is right for them are also vital. “[We need] more and cheaper availability of abuse deterrent opioids, and making effective treatments like buprenorphine more available from competent prescribers who are willing to have more than 100 patients under their care,” Kosten says.
While it’s devastating that Prince was so close to being administered buprenorphine, the reality is that for many Americans living in addiction, buprenorphine remains hardly an option at all. Dr. David Kessler, a former commissioner of the Food and Drug Administration, said today, “We need to see the Prince in all of us. We need to see the vulnerability. We’re all vulnerable here. It’s a wakeup call for how we view these drugs.”